This extreme version of PMS can be both life-changing and life-threatening. How can birth control help in alleviating symptoms of PMDD?
Premenstrual Dysphoric Disorder (PMDD) is more than just Premenstrual Syndrome (PMS)
For starters, PMDD is not a hormonal imbalance nor is it merely behavioural changes during that excruciating time of the month!
PMDD is commonly defined as an endocrine disorder and is also known to be a more severe form of PMS. They are both similar in terms of experiencing hormone-related symptoms in physical and emotional forms. This typically happens during the premenstrual phase about seven to 10 days before your period starts, and persists for the first few days of your period.
While this may sound familiar to most women (and significant others or partners who have to bear the brunt of PMS every month), there is a huge difference between PMS and PMDD. In fact, PMDD can be so extreme that sudden shifts in mood can disrupt daily life and even negatively affect relationships. In some cases, besides facing challenges in interpersonal functioning and maintaining social relations, PMDD can also cause occupational impairment. This may refer to frequent outbursts towards loved ones or the inability to cope with the distressing symptoms at work, ultimately requiring one to take medical leave.
How serious is PMDD?
PMDD affects about 5 percent of women of reproductive age and those who have underlying depression and anxiety are more likely to suffer from it. While there is no clear cause for this disorder, possible causes include genetics, thyroid and detrimental factors such as alcohol and substance abuse.
According to the manual for assessment and diagnosis of mental disorders DSM-5, PMDD is also defined as a depressive disorder that requires prescription medication, unlike PMS. As its effects on women’s mental health are consistent and yet intermittent, PMDD tends to be underdiagnosed and undertreated. Thus, although PMDD may be uncommon compared to PMS, it is important to render conscientious attention and treatment as symptoms may worsen over time especially upon entering into menopause. As such, those with PMDD may harbour suicidal thoughts and behaviour which can be life-threatening.
What are the symptoms of PMDD?
Similar to PMS, PMDD also causes bloating, breast tenderness, fatigue and changes in diet and sleeping habits. But the display of at least one of the below emotional and behavioural traits differentiates PMDD from PMS:
- Feeling sad or hopeless
- Severe moodiness
- Anxiety or tension
- Easily irritable or angry
If you experience either one of the symptoms alongside other common symptoms* which occur before your menstrual flow that significantly disrupts your ability to function in everyday life, there is a chance you may be suffering from PMDD.
| Emotional Symptoms | Physical Symptoms |
| – Agitation or nervousness – Irritability – Feeling overwhelmed and out of control – Crying spells – Anger, sadness – Suicidal thoughts – Panic attacks, paranoia – Moodiness – Forgetfulness – Loss of interest in activities and relationships | – Acne – Back, joint or muscle pain – Bloating – Breast swelling and tenderness – Constipation, diarrhoea, nausea, vomiting – Cramps – Dizziness, headaches – Appetite changes – Reduced sex drive – Lethargy or fatigue – Sleep disturbance |
If you feel you check most of these boxes, you can first take a self-screening test online. As PMDD symptoms may overlap with features of other medical conditions that mimic PMDD, it is strongly advised to seek professional help and speak with a healthcare provider for a diagnosis thereafter.
How can birth control help with PMDD?
Yes, birth control does more than helping you prevent pregnancy!
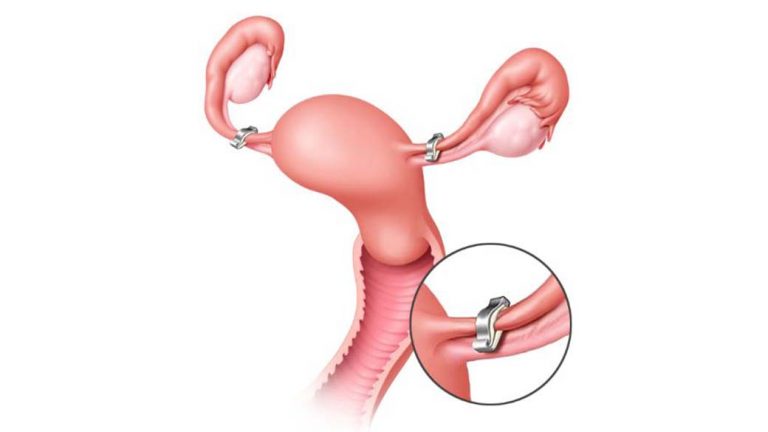
Hormonal interventions utilising oral contraceptives is one useful method in treating both PMS and PMDD. PMDD symptoms tend to arise once ovulation begins. Thus, as birth control pills prevent ovulation, they can regulate hormone levels in order to suppress ovulation and its related hormone changes, thereby avoiding premenstrual symptoms.
Most birth control pills are usually prescribed such that there are 21 active pills followed by seven days of placebo pills containing only sugar. This creates a hormone-free interval where the transition from taking active pills to sugar pills causes a sudden decrease in hormones.
Currently, Yaz is the only FDA-approved hormonal birth control pill used to treat PMDD. It implements a 24-day dosing regimen with active pills, followed by four inactive sugar pills. Similarly, other birth control options such as contraceptive patches and rings can also help to treat PMDD.
Nonetheless, these benefits are also accompanied by certain risks for some individuals. Some may be more sensitive toward the sudden fluctuations in hormone levels and instead experience even more severe mood swings. Unsuitable candidates for treating PMDD with hormonal medications also include:
- Those with a past medical history of blood clots, stroke or migraine
- Smokers, especially those over 35 years of age
What are other treatment options or alternatives?
More often than not, a combination of solutions is needed in order to treat PMDD.
Other ways to prevent or minimise PMDD symptoms:
- Selective serotonin reuptake inhibitors (SSRIs) — commonly prescribed antidepressants
- Nutritional supplements rich in calcium
- Over-the-counter pain relievers such as ibuprofen and aspirin to relieve physical symptoms
- Stress management
What’s next? Well, taking charge of your own health and wellness is also extremely important in treating PMDD. Firstly, you can start with small steps such as having frequent meals lower in salt but high in nutrients from fruits, vegetables and whole grains. Next, have sufficient hours of sleep or try out various relaxation techniques like meditation and yoga.
Exercising five days a week for at least half an hour a day and cultivating healthy sleep habits will also aid in reducing premenstrual symptoms. And if you’re a coffee addict or frequent bar-goer every TGIF, perhaps it’s time to cut down on both the caffeine and alcohol as they will also help to ease symptoms.
Remember, you can take charge!
Ultimately, it is always important to get the right diagnosis if you feel like you have PMDD. So here’s an important tip: A tracking journal will be most useful for you to start tracking and recording your symptoms before you decide to visit the doctor. Different remedies may work differently for every individual but if you do decide to opt for birth control as a solution, don’t hesitate to find out more about your options with Siena!
References:
- Burnett, T. (2021, March 11). Premenstrual dysphoric disorder (PMDD): A severe form of PMS. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/premenstrual-syndrome/expert-answers/pmdd/faq-20058315.
- Chen, H. (n.d.). Premenstrual Dysphoric Disorder (PMDD): When PMS gets severe. HealthXchange.sg. https://www.healthxchange.sg/women/urology/premenstrual-dysphoric-disorder-pms-severe.
- Hormone Health Network. (2018, August). Premenstrual Syndrome and Premenstrual Dysphoric Disorder. https://www.hormone.org/diseases-and-conditions/pms-pmdd
- International Association for Premenstrual Disorders. (n.d.). PMDD/PME Self-Screen. https://iapmd.org/self-screen.
- Mayo Foundation for Medical Education and Research. (2019, September 17). The most commonly prescribed type of antidepressant. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/depression/in-depth/ssris/art-20044825.
- Raffi, E. R. & Freeman, M.P. (2017). The Etiology of Premenstrual Dysphoric Disorder: 5 Interwoven Pieces. Current Psychiatry, 16(9), 20-28.
- The MGH Center for Women’s Mental Health. (n.d.). PMDD/PMS: When PMS symptoms interfere with functioning & quality of life. https://womensmentalhealth.org/specialty-clinics/pms-and-pmdd/.






:max_bytes(150000):strip_icc()/GettyImages-1081205870-52fb358b5ca148abb8d35d48b1f7ffb7.jpg)