Periods can be tough. Most of us learn (the hard way) that it’s pretty much impossible to avoid both the physical and emotional symptoms of your menstrual cycle. From painful menstrual cramps to bloating, fatigue and irrational mood swings, there are seriously tons of reasons validating that dreadful feeling you get when you’re on your period.
But you’re definitely not alone. Approximately 80 percent of women experience period pain (dysmenorrhoea) in their lifetime and in 5 to 10 percent of women, the pain can be so severe that it disrupts their daily life. While some of those who experience dysmenorrhea rely on over-the-counter painkillers, others may also seek longer-term remedies like birth control to help reduce the pain associated with menstrual cramps.
Looking for an everyday solution that’s more convenient and perhaps even free? Try these easy period hacks that can help you cope better during that time of the month!
Dietary Changes
Snuggling in bed with junk food on both hands, Netflix and a pint of ice-cream waiting by your bedside. Yes, I’m sure we’ve all been there in one way or another. It can get really tempting to just wait out your period in the most comforting (yet unhealthy) manner possible.
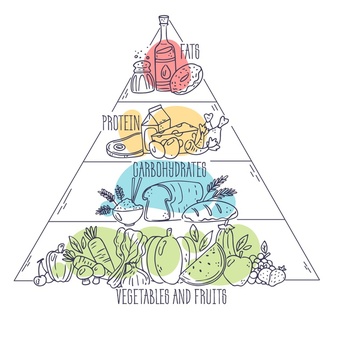
1. Stay away from simple carbs, sugar and salt
Of course, along with your period also comes the time you’re most likely to indulge in food high in carbohydrates, sugar and salt. Mostly because you feel like it. However, they can actually cause energy levels to crash whilst intensifying mood swings and bloating due to higher water retention.
Instead, try to consume protein-rich foods and those with healthy fats and high fibre which can help to stabilise your blood sugar levels and decrease inflammation. Or you could also consider having more complex carbs found in wholegrain food as they keep you full longer, thus reducing your food cravings and irritability.
2. Hydrate
Drink up (water, not alcohol)! Having plenty of water helps with digestion, hormone regulation and hydration. Research has shown that staying hydrated (at least 1600ml a day) can decrease the duration of menstrual bleeding and the severity of menstrual pain.
If you’re usually reliant on that cup of espresso to kickstart your days or plenty of nights with at least one glass of wine, it might be a better idea to avoid them around the time of your period. Both caffeine and alcohol have the potential to enhance premenstrual syndrome (PMS) symptoms such as irritability, restlessness and tension.
3. Don’t forget your daily nutrients/supplements
Calcium is a key dietary intake that can help relieve PMS symptoms like depression and fatigue. In the week leading up to your period, you might want to consider stocking up on milk, other dairy products and even cereal.
When taken together, magnesium and vitamin B-6 are most effective in helping you cope with symptoms like depression, anxiety, bloating and food cravings. Vitamin B-6 is commonly found in fish, chicken and fruits while you can also expect to have magnesium in your leafy greens like spinach, and in whole grains and nuts.
Lifestyle Recommendations
Dating back to your teenage years, you might already be accustomed to a certain routine or way of life when it comes to your period. Good on you if it’s been working well for you so far! But for those of you still on the lookout for ways to improve your period health, it’s best to re-evaluate your current lifestyle and learn from some of the tips below.
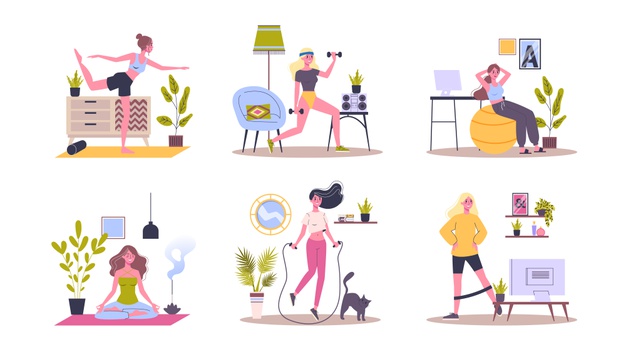
1. Get up and get moving
No matter how much you feel like it, don’t let yourself become a couch potato!
Be it hiking, jogging, biking, dancing or even as simple as taking a stroll, any kind of exercise for at least 30 minutes a day can do you good. As long as it gets your heart pumping, the release of mood-boosting endorphins is a great way to improve PMS symptoms like fatigue, poor concentration and depression.
2. Quality sleep
Feel like you’re getting enough hours of sleep but can’t fathom why you still wake up feeling grouchy and moody? Well, here’s a plausible explanation.
As you may find it harder to fall asleep at night whilst enduring your period symptoms, any disruption to your sleep pattern can also increase your irritability and even cause menstrual migraines. To tackle this, try sticking to a sleep routine where you head to bed at the same time each night and wake up at the same time in the morning.
Turn in earlier by reducing your screentime in bed so that you’ll also have the full, minimum eight hours of sleep. This will not only help to rejuvenate you, but it also stabilises your hormones.
3. Break your habit
Smoking can lead to more severe PMS symptoms and menstrual problems like cramping and irregular periods. This happens because it alters your hormone levels and even lowers plasma vitamin D levels which potentially increases the incidence and/or severity of PMS.
At-Home Care and Relaxation Techniques

Sometimes, all you really need during the few days of menstruation is to relax and forget about your troubles and worries. That’s all there is to it, period.
1. Therapeutic care
It can be stressful juggling your life’s commitments and daily activities, alongside your period. But fret not, there are so many relaxation techniques you can adopt to wind down and give yourself the self-care you deserve.
Yoga is one effective activity for your stress management as the combination of gentle movements and deep breathing techniques help to relax your muscles and improve blood supply to the pelvic area. A study found that doing regular yoga exercises actually improved PMS bloating, cramps and sore breasts, hence decreasing premenstrual distress.
Alternatively, a back and stomach massage could also be another solution for you to calm your nerves and anxiety around the time of your period, as well as to ease physical discomfort. An hour of massage can reduce your cortisol levels — a hormone triggered in times of stress — and produce a feel-good chemical, serotonin. This boosts your body’s ability to deflect pain, anxiety and negative emotions.
2. Turn up the heat
Warm-anything is the way to go during your period! They help relax the muscles of your uterus causing period cramps and also boost circulation in your abdomen.
These are some simple and effective ways to ease tension and for pain relief:
- Soak in a warm bath with aromatherapy oils
- Use a heating pad, patch or wrap
- Hug a hot water bottle
- Enjoy a cup of hot ginger tea
3. Stay positive
More often than not, taking care of your mental health may be just the thing to beat the period blues (emotionally at least). And these are probably the most basic of tips that some of you may have overlooked!
We cannot emphasise enough how important rest is. Periods are obviously exhausting so don’t feel guilty for taking all the rest you need to recharge.
If you’re tucked in bed feeling lonely and horrible, try listening to audiobooks and podcasts, or simply reach out to a friend or loved one to chat about what’s on your mind.
And if you’re up for it, why not learn something new or invest your energy into a task you’ve been wanting to take on? Make yourself a new smoothie recipe, spend a few minutes on the piano or simply rearrange your bookshelf if it makes you feel better. You’ll probably feel the tiniest sense of accomplishment and satisfaction while getting a whole lot of inspiration in time for your post-period activities!
Should You See A Doctor?
With plenty of period hacks to choose from, you’ll hopefully get better at managing your next and subsequent menstrual cycles! While they may not work for everyone, your period problems will most likely be more tolerable whenever the dreaded time of the month rolls around. Just remember to stick to the ones that work best for you and don’t be afraid to experiment.
However, if your PMS symptoms are seriously unbearable and extreme such that it severely disrupts your daily life, consider seeking professional help from a doctor. With Siena, all you have to do is fill up a questionnaire to schedule a tele-consult with one of our female doctors to discuss the complications and find relief from your PMS symptoms — all from the privacy and comfort of your own home.
Summary
How To Relieve Period Cramps?
- Dietary Changes
Cut down on simple carbs, sugar and salt, constantly hydrate and don’t forget your daily nutrients & supplements.
- Lifestyle Recommendations
Exercise, have sufficient quality sleep and stay away from bad habits like smoking.
- At-Home Care and Relaxation Techniques
Indulge in therapeutic care such as yoga and massage, use heat pads or take a warm bath while staying positive.
References:
- Bertone-Johnson, E. R., Hankinson, S. E., Johnson, S. R., & Manson, J. E. (2008). Cigarette Smoking and the Development of Premenstrual Syndrome. American Journal of Epidemiology, 168(8), 938–945. https://doi.org/10.1093/aje/kwn194.
- Boyle, N.B., Lawton, C., & Dye, L. (2017). The Effects of Magnesium Supplementation on Subjective Anxiety and Stress — A Systematic Review. Nutrients, 9(5), 429. https://doi.org/10.3390/nu9050429.
- Gupta, P. (2019, November). Period Pain. Women’s Health Concern. https://www.womens-health-concern.org/wp-content/uploads/2020/12/20-WHC-FACTSHEET-Period-Pain-DEC2020.pdf.
- Mayo Clinic. (2014, June 25). Can massage relieve symptoms of depression, anxiety and stress? https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/can-massage-relieve-symptoms-of-depression-anxiety-and-stress.
- Torkan, B., Mousavi, M., Dehghani, S., Hajipour, L., Sadeghi, N., Ziaei Rad, M., & Montazeri, A. (2021). The role of water intake in the severity of pain and menstrual distress among females suffering from primary dysmenorrhea: a semi-experimental study. BMC Women’s Health, 21(1). https://doi.org/10.1186/s12905-021-01184-w.
- Tsai, S.-Y. (2016). Effect of Yoga Exercise on Premenstrual Symptoms among Female Employees in Taiwan. International Journal of Environmental Research and Public Health, 13(7), 721. https://doi.org/10.3390/ijerph13070721.