Feel like you never get your periods? Or when you do get them, it seems like there’s no end to it? Well, you may be suffering from a condition called polycystic ovary syndrome (PCOS) that affects your hormone levels.
What is Polycystic Ovary Syndrome (PCOS)?
PCOS is a common hormonal disorder that affects approximately 10% of women who are of reproductive age. The infrequent or prolonged menstrual periods caused by excess male hormones or androgen levels are one of the most obvious signs of PCOS.
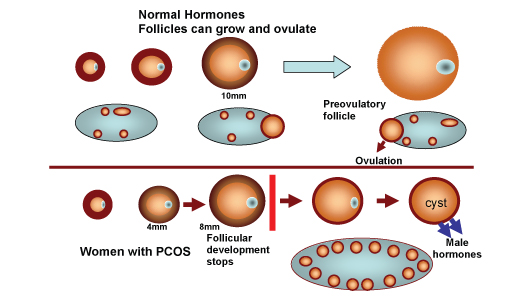
Those suffering from PCOS have an imbalance of female hormones that prevents their ovaries from releasing an egg monthly. As a result, the ovaries end up developing countless small collections of fluid sacs (follicles) and fail to regularly release eggs. Each sac contains an immature egg that is unable to mature enough to trigger ovulation.
You may be wondering where the term “polycystic” comes from. As the unreleased eggs remain in the ovaries, these multiple small cysts contribute to the polycystic appearance of the ovaries.
Essentially, by also producing higher-than-normal amounts of male hormones leading to hormonal balance, this causes your body to skip menstrual periods and makes it harder for you to get pregnant.
Signs and Symptoms of PCOS
Signs and symptoms of PCOS often develop during puberty, around the time you go through your first menstrual cycle. However, PCOS can also develop at a later stage due to substantial weight gain.
You’ll definitely want to pay attention to:
- Irregular periods: could be infrequent, prolonged or even absent
- Heavy bleeding
- Hair growth
- Acne
- Weight gain
- Male-pattern baldness
- Darkening of the skin
- Headaches
If you think you have PCOS, you should observe and track your periods as they are usually the most common signs.
Other symptoms that may be more obvious are associated with physical changes. These refer to excess facial and body hair, severe acne and male-pattern baldness as they signify the presence of excess androgen in your body.
Severe symptoms usually arise if you’re obese.
Causes of PCOS
So far, the exact cause for PCOS is unknown although it may be hereditary as research suggests genes also contribute to PCOS.
But the most commonly cited reason is probably excess male hormones called androgen. Women normally produce androgen in small quantities but for those with PCOS, they produce an excessive amount which explains the male-pattern hair growth (i.e. on the chin, chest, inner thighs, etc) and the formation of acne. When your ovaries produce abnormally high levels of androgen, you can also gain weight both easily and quickly.
Some studies have also shown that excess insulin increases androgen production which contributes to PCOS. Insulin is the hormone produced in your pancreas allowing cells to use sugar and also acts as your body’s primary sugar supply. If your cells become insulin-resistant, your blood sugar levels can rise thus causing your body to produce more insulin.
How is PCOS Diagnosed?
A diagnosis of PCOS is made when you experience at least two of these signs:
| Irregular periods | – Infrequent, irregular or prolonged menstrual cycles are the most common signs of PCOS. – A good gauge would be: if you have fewer than nine periods a year, more than 35 days between periods and abnormally heavy periods. |
| Excess androgen | Elevated levels of male hormones (androgen) may cause physical changes like excess facial and body hair (hirsutism), occasionally severe acne and male-pattern baldness. |
| Polycystic ovaries | Enlarged ovaries that contain follicles surrounding the eggs. Thus, the ovaries may not be able to function regularly. |
Other ways to diagnose PCOS:
- Hormonal blood tests
- By analysing your blood to measure your hormone levels, you can then safely exclude other plausible causes like menstrual abnormalities or merely androgen excess mimicking PCOS.
- Pelvic ultrasound scan
- Examine the appearance of your reproductive organs and the thickness of your uterine lining.
Targeted Treatments To Cope With PCOS
PCOS is not completely reversible but several treatments can help reduce or minimise uncomfortable symptoms, allowing you to better cope with the condition.
Birth control for irregular periods and its related symptoms
Already on birth control? Well, you may be killing two birds with one stone if you’re currently struggling with PCOS too.
Combined hormonal contraceptives are usually prescribed to control various PCOS symptoms. Some examples are the combined birth control pill, patch and even the vaginal ring. The estrogen and progestin hormones present in the hormonal birth control help decrease androgen and regulate estrogen levels instead.
To treat irregular periods (a common PCOS symptom), combined hormonal contraceptives are also recommended to aid in fixing hormonal imbalance and regulating the menstrual cycle.
What’s more, regulating hormones can even lower your risk of endometrial cancer and correct abnormal bleeding, excess hair growth and acne!
Clomiphene or surgery for infertility
The irregular and infrequent ovulation caused by PCOS can make it difficult for you to conceive. So if you’re planning for a baby or if you intend to get pregnant in the near future, it’ll definitely be useful to know that ovulation can be artificially induced using medications.
A common drug used to induce ovulation is clomiphene (Clomid) which has to be taken orally for five days. If the tablet fails, you may need to consider hormone injections to stimulate the ovaries. But of course, this depends on the recommended treatment plan based on professional advice and guidance from your doctor or specialist.
If you find that your body is unresponsive to medical treatment, there’s also the option for surgery. Laparoscopic ovarian drilling is typically used to trigger ovulation by using electrocautery or a laser to destroy parts of the ovaries. This corrects hormonal imbalance and restores normal ovulation.
Hair removal medications for excessive hair growth
Excess hair may be something you’re not used to and find frustrating when you experience PCOS symptoms. Several fuss-free and convenient techniques include depilatory creams, shaving, waxing, bleaching, plucking and electrolysis. However, these methods have to be sustained or repeated in order to manage hair growth.
Suppression of male hormone production with tablets like the oral contraceptive pill or anti-male hormone drug may also reduce excessive hair growth if used for at least nine months.
Lastly, you can also consider laser hair removal as it’s the most effective long-term method to help tackle the problem of excess hair. However, it’s probably one of the most expensive options as well.
Lifestyle changes
As substantial weight gain has also been attributed to PCOS, paying attention to your diet and regularly exercising to reduce excess weight may help to improve symptoms by restoring normal hormonal balance.
To do so, you can also limit your intake of carbohydrates to increase insulin levels, or opt for food high in complex carbohydrates (e.g. whole grains and vegetables) to gradually raise your blood sugar levels.
The Bottom Line
If you suspect you have PCOS, it’s really important to seek timely and appropriate treatment to prevent further complications. That said, always seek help from your doctor first to figure out the best approach or course of treatment for your body and lifestyle.
Considering birth control? Here at Siena, we also want to help you find a solution to help you manage your PCOS symptoms. If you’re considering birth control, don’t hesitate to reach out and book a consult with one of our female doctors to explore your options!
References:
- Diamanti-Kandarakis, E., Kandarakis, H., & Legro, R. S. (2006). The Role of Genes and Environment in the Etiology of PCOS. Endocrine, 30(1), 19–26. https://doi.org/10.1385/endo:30:1:19.
- Galan, N. (2020, November 25). The Link Between PCOS and Insulin Resistance. Verywell Health. https://www.verywellhealth.com/pcos-and-insulin-resistance-2616319.
- Mayo Clinic. (2020, October 3). Polycystic Ovary Syndrome (PCOS). https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439.
- National University Hospital. (n.d.). Polycystic Ovary Syndrome. https://www.nuh.com.sg/Health-Information/Diseases-Conditions/Pages/Polycystic-Ovary-Syndrome.aspx.
- Watson, S. (2021, April 19). Polycystic Ovary Syndrome (PCOS): Symptoms, Causes and Treatment. Healthline. https://www.healthline.com/health/polycystic-ovary-disease.