Do you find it difficult to remember to take a pill every day? Do you have difficulty swallowing pills?
If you answered yes to any of the above questions, the birth control patch could be a viable option for you! Both birth control pills and patches use hormones to prevent pregnancy, but the way the hormones are delivered differs. You apply the patch to your skin once a week and forget about it.
In this article, we share all you need to know about the EVRA® Transdermal Patch. Read on to learn more about:
- How it works;
- How to use it;
- What to do if you missed a patch;
- Potential side effects; and
- How to buy EVRA® Transdermal Patch in Singapore.
What Is EVRA® Transdermal Patch?
The EVRA® Transdermal Patch is a small, beige sticky patch that contains 2 hormones:
- Progestin (6mg norelgestromin); and
- Estrogen (0.6mg ethinyl estradiol).
The patch works by releasing hormones into your body through your skin to prevent pregnancy.
The patch is mainly used as contraception to prevent pregnancy. However, women using the EVRA® Transdermal Patch may also benefit from the non-contraceptive effects of estrogen such as:
- Regulate or lighten menstruation
- Prevent anaemia by making periods lighter or shorter
- Lessen menstrual cramps (dysmenorrhea)
- Manage symptoms of premenstrual syndrome (PMS) and premenstrual dysmorphic disorder (PMDD)
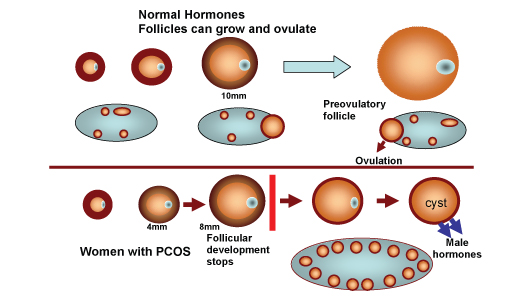
- Treat symptoms of polycystic ovary syndrome (PCOS)
- Treat endometriosis or uterine fibroids
- Lower the risk of ovarian cancer, uterine cancer and colon cancer
- Improve acne
- Stop unwanted hair growth
- Reduce migraines
- Control hot flashes during the transition into menopause
How Does EVRA® Transdermal Patch Work?
After the patch is in place, it delivers a steady dose of hormones through your skin and into your bloodstream.
EVRA® Transdermal Patch prevents pregnancy by:
- Inhibiting ovulation, the release of an egg from the ovary;
- Thickening the cervical mucus (the fluid in the vaginal tract), such that it is hard for the sperm to reach the egg to fertilise it;
- Thinning of the uterine lining, such that even if an egg is fertilised, it will be unable to attach to the uterus. The fertilised egg will instead be passed out of the body.
How Effective Is EVRA® Transdermal Patch?
When used perfectly, EVRA® Transdermal Patch is more than 99% effective in preventing pregnancy. It is typically 91% effective (in events of missed applications or improper storage etc.), according to a report by the Centers for Disease Control and Prevention.
Birth control patches are generally more effective than male condoms in preventing pregnancy — male condoms are 98% effective when used perfectly, and 82% effective in typical use. However, it is important to note that birth control patches do not protect women against sexually transmitted infections (STIs), unlike male condoms.
Therefore, it is recommended to use dual protection of condoms and non-barrier contraceptives such as birth control patches during any sexual activity.
How To Use EVRA® Transdermal Patch?
Each pack of EVRA® Transdermal Patch contains 3 patches. Apply your first patch and wear it for 7 days. On day 8, change the patch to a new one. Change the patch every week for 3 weeks, and then have a patch-free week.
During your patch-free week, you’ll get a withdrawal bleed, like a period, although this may not always happen.
After 7 patch-free days, apply a new patch and start the 4-week cycle again. Start your new cycle even if you’re still bleeding.
Where to put the patch:
- Always put your patch on clean, dry and hairless skin.
- Put it on the buttock, abdomen, upper outer arm or upper back.
- Put it on places where it won’t be rubbed by tight clothing.
- Do not put on the breast or waistline, and on any open wounds, cuts or irritated skin.
- Do not use adhesive or wraps to hold the patch in place.
- Do not use creams, oils, lotions, powder or other skin care products on the application site. The patch may not stick well.
How to open the patch:
- Open the foil sachet by tearing it along the edge with your fingers.
- Peel away half of the clear protective covering without touching the sticky surface.
How to put the patch:
- Put the patch on your skin and remove the other half of the protective covering.
- Press down firmly on the patch with the palm of your hand for 10 seconds, making sure the edges stick well.
What To Do If The Patch Becomes Loose, Lifts At The Edges Or Falls Off?
Usually, the patch remains sticky, even if you get sweaty while exercising or take a shower. On rare occasions where the patch loosens (less than 3% of patches) or falls off (less than 2% of patches), you can follow the below steps to ensure you are still protected against pregnancies.
For less than 48 hours:
- Try to put the same patch on again or put on a new patch immediately if:
- it is no longer sticky;
- it has become stuck to itself or on another surface or material; or
- it is the second time it has become loose or has fallen off.
- Change your patch on your normal change day.
- You’re protected against pregnancy if you’ve used your patch correctly for the past 7 days (and the 7 days before your patch-free week, if you’re in week 1).
For 48 hours or more, or if you are unsure of the duration:
- Put on a new patch immediately.
- If you’re in week 1 or 2 of your patch cycle, change your patch on your normal change day.
- If you’re in week 3, you need to start a new patch cycle (this is now day 1 of your new cycle) and skip your usual patch-free week.
- Consider taking emergency contraception if you had unprotected sex in the last 7 days.
- Use extra contraception (i.e. condoms) or abstain from sex until you’ve had a patch on for 7 days in a row.
What To Do If I Forget To Change My Patch?
If you forget to change your patch for one to two days (up to 48 hours):
- Put on a new patch as soon as you remember.
- Change your patch on your normal change day.
- A barrier method of contraception is not needed.
If you forget to change your patch for more than two days (48 hours or more):
- Start a new four-week cycle as soon as possible.
- Consider taking emergency contraception if you had unprotected sex in the last 7 days.
- Use extra contraception (i.e. condoms) or abstain from sex until you’ve had a patch on for 7 days in a row.
If you forget to take off your patch (at Week 4):
- Take it off as soon as you remember.
- Start your next cycle on your normal “Patch Change Day”, the day after Day 28.
- A barrier method of contraception is not needed.
If you forget to take off your patch (after Week 4):
- Take it off as soon as you remember.
- Put on the first patch of your new cycle as soon as you remember.
- Use extra contraception (i.e. condoms) or abstain from sex until you’ve had a patch on for 7 days in a row.
- You now have a new “Patch Change Day” and new Day 1.
What Are The Potential Side Effects Of EVRA® Transdermal Patch?
Women who just started using EVRA® Transdermal Patch may experience some of the following side effects:
- Nausea and bloating. Taking the medication after food may help reduce these side effects.
- Headache. Taking over-the-counter painkillers such as Paracetamol may help manage the pain.
- Vaginal bleeding between periods (spotting).
- Breast soreness.
- Mood changes.
These symptoms vary among individuals and normally subside within 2-3 months as your body starts to get accustomed to the changes in hormone levels. Do inform your doctor if you experience any of these symptoms for longer than expected or if they are bothering you.
How To Buy EVRA® Transdermal Patch In Singapore?
Birth control patches are prescription-only medicines in Singapore. You would need to consult a doctor in person before you can get started on any birth control.
With Siena, you can have access to affordable birth control without leaving home. Simply complete an online questionnaire, and speak with a doctor online. If prescribed, your medication will be delivered to you in discreet packaging and at no additional charge.
References
- Centers for Disease Control and Prevention. (2014, April). Appendix D: Contraceptive Effectiveness. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6304a5.htm
- SingHealth. (2017, October). Evra Transdermal Patch. https://www.singhealth.com.sg/patient-care/medicine/evra-transdermal-patch